Cracks in our health care system have become chasms during the COVID-19 pandemic, highlighting inequities, expanding wait times and further straining an already burdened system. How can we build a better health care system that serves all Canadians?
“As health advocates, we must seize this moment when change is needed most.”
— Dr. Ann Collins, CMA president
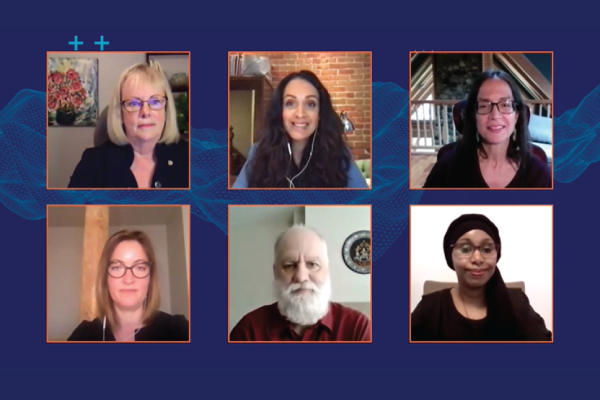
This question helped guide the first virtual 2021 CMA Health Summit session, bringing together physicians, medical learners, policy-makers and patients across Canada.
While COVID-19 created opportunities for innovation — including the expansion of virtual care and collaboration between often siloed areas of health care — the pandemic underscored the system’s severe vulnerabilities.
“Everything we learned from the experience of COVID-19, truly we already knew.”
— Dr. Danielle Martin, keynote speaker and executive vice-president at Women’s College Hospital
Both Dr. Martin and fellow keynote speaker Dr. Nadine Caron emphasized the need to strengthen primary care services and address social determinants of health.
“With COVID-19 we recognize that poverty and employment … continue to be major drivers,” said Dr. Caron, a member of the Sagamok Anishnawbek First Nation and a surgical oncologist serving individuals in rural, remote and northern BC.
Panellist and patient advocate Sudi Barre shared her personal story of recovering after giving birth, only to experience a series of heart attacks and strokes — the result of the potentially fatal condition spontaneous coronary artery dissection (SCAD). Barre, who is of Somali descent, shared the difficulties she faced during her rehabilitation, including her inability to take time off work because of the financial strain of treatment. “What women receive is not universal health care, it just isn’t,” she said, noting that challenges are compounded for racialized women.
Panellist and Globe and Mail health columnist André Picard talked about the shift that is needed to better care for seniors. “It begins with a philosophy of valuing the elderly and wanting them to remain in the community,” he said.
Following the panel discussion — moderated by journalist Althia Raj — summit participants joined small breakout groups to discuss topics including how to better serve marginalized groups and how to overhaul health care to improve social supports.
One participant summed up their breakout session this way: “We have an incredibly reactionary system — moving forward, an emphasis on addressing the upstream determinants and reasons people become ill will help save resources and time in the long run.”
Other discussions focused on ensuring a patient-partnered approach and communicating effectively with communities about their medical needs. For one participant, who has spent the last year working in a COVID-19 unit, that means improving translation services at hospitals for patients who do not use English or French as a first language.
Dr. Collins wrapped the session by acknowledging the value of the ideas brought forward and the opportunities to build on the positive changes to the health care system made during the pandemic, through the CMA’s Impact 2040 strategy.
.
