It’s tempting to treat the health workforce crisis as a math problem.
In the first quarter of 2022, there were 136,800 health sector employment vacancies across Canada – an all-time high. Every one of them affects thousands of patients. And as the pandemic has underscored, a labour shortage in one area – a doctor’s early retirement or a nurse on sick leave – affects capacity everywhere else.
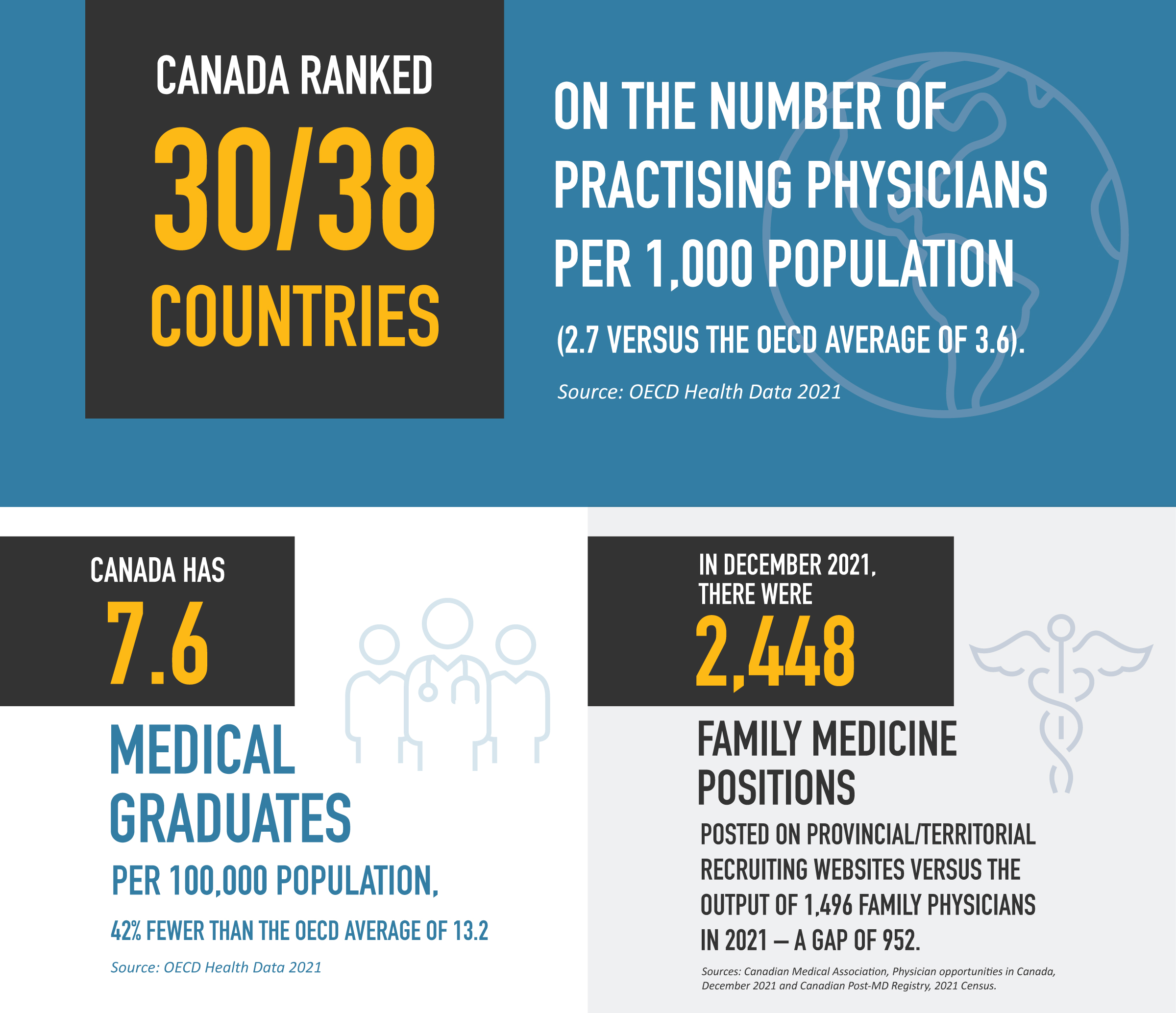
More health workers are urgently needed. Providers are experiencing unprecedented exhaustion, burnout and job dissatisfaction. Patients are not getting the care they need.
But the health workforce needs bolder action than addition – it requires coordinated national planning for the right kind of care, in the right places, at the right times.
Current health workforce planning is siloed, focused on one profession in a single region. This patchwork also tends to ignore changing professional lifespans, demographics and population health needs.
We need a planning framework that reflects the reality of complex, interdependent health care labour markets. We need to create environments where people want to work and where workloads are manageable.
And we need to start now.
Although short- and medium-term tactics are critical to stabilize the health system, we cannot build a thriving health workforce – the foundation of sustainable, accessible care – without integrated long-term planning.
We definitely need to address our health human resource challenges. We don’t have enough physicians, nurses and many other health care providers to meet the needs of Canadians in our current way of working.
– Dr. Kathleen Ross, CMA president
Learn how expanding team-based care can help
The integration of health human resources planning requires integrated advocacy.
The Canadian Medical Association (CMA) is bringing together many different players – professional and patient associations, educational institutions, regulatory bodies, health organizations, and all levels of government – to discuss and develop a national planning framework. Although our work is still at an early stage, working in allyship with First Nations, Inuit and Métis providers and communities is also critical to ensure equitable health outcomes.
Our vision is a health workforce coordinated across health disciplines and specialties, geography, funding models, population health needs – and rooted in core principles of equity and Reconciliation.
At the CMA, we believe a cohesive approach to workforce planning is essential to building a better future of health:
- Overlaying population health and demographic data would allow provinces to anticipate, adapt and better deploy the health workforce to meet unique population needs
- Shared labour market data across jurisdictions would provide a national snapshot of projected retirements and attrition and enable educational institutions to tailor enrolment levels and training mixes to hiring needs.
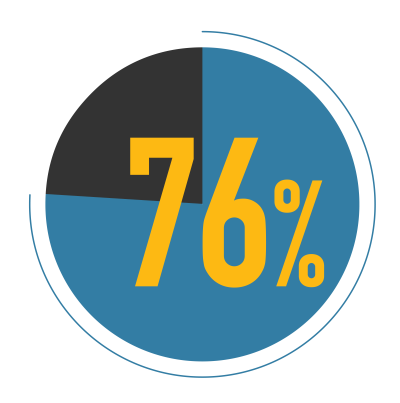
76% of Canadians believe Canada doesn’t have the right number of health workers across all regions.
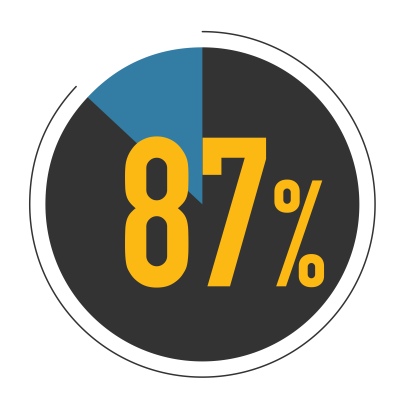
87% of Canadians want a long-term plan for the health workforce to ensure the right care, at the right time, wherever they live.
Source: Ipsos/CMA survey, September 2023
Integrated health workforce planning would also support team-based care and inter-professional collaborations – improving outcomes for patients navigating an increasingly complex health system as well as addressing the increasing burden of administration and staff shortages on providers and empowering them to work to optimal scope of practice.
Here's what we don't know about health care in Canada
If we have a better picture of what health care in Canada looks like – what the needs are – not only now but in the future, this will help retain and attract the future workforce to fill them.
– Dr. Dax Bourcier, Medical resident
Our work on an integrated health care workforce
The CMA partnered with the CNA and the College of Family Physicians of Canada (CFPC) to develop eight recommendations for federal investments to help alleviate the workforce crisis and prevent more of them in the future.
Along with the CNA, we recommended that the House of Commons Standing Committee on Health undertake a study on the health workforce crisis, which they’ve since done.

The joint recommendations were also presented to the Federal/Provincial/Territorial Committee on Health Workforce – the first time in more than a decade that the CMA had presented to this committee. The federal government has advanced one of the recommendations – to invest in programs that will allow internationally educated health professionals to get licensed in Canada to fill vacancies.
In October 2023, the CMA attended the in-person meeting of Canada’s Health Ministers in Charlottetown to call for change – and government responded. Coming out of their meeting, the health ministers committed to supporting the country’s health workforce by scaling up physician mobility, providing more training opportunities, improving the availability and sharing of labour market data, and expediting credentials for internationally trained health professionals.
Our partners on health workforce reform
The CMA works closely with the profession as well as our Patient Voice members. In October 2023, we brought together more than 40 national and provincial health organizations to co-create solutions to Canada’s health workforce crisis.
The CMA is also participating in the following groups:
-
The steering committee of the Centre of Excellence for the Future of the Health Workforce, led by the Canadian Institute for Health Information
-
The Canadian Academy of Health Sciences Assessment on Health Human Resources
-
Health Canada’s Coalition for Action for Health Workers, which will inform immediate and longer-term solutions to address employment challenges
-
The HEAL Health Human Resources task force
With funding from a CMA Foundation grant, McMaster Health Forum is also bringing together organizations and citizens – including members from CMA Patient Voice – in a series of dialogues and panels.
When calculating future health human resource needs, serving all patients needs to be an integral part of the equation – including for those who avoid the health care system for very valid reasons.
– Michelle Hamilton-Page, CMA Patient Voice member and 2SLGBTQI advocate
What physicians can do to help
Collaboration with physicians and learners of all ages, stages and specialties, from rural and remote communities as well as big cities, is essential for a better way forward.
