How bad is it?
We know that health care professionals have experienced profound stress through the COVID-19 pandemic. Physicians are talking openly about burnout, exhaustion, moral distress — and, not surprisingly, a growing exodus from the profession of medicine.
The CMA’s latest National Physician Health Survey (NPHS) now fills in that picture with troubling detail.
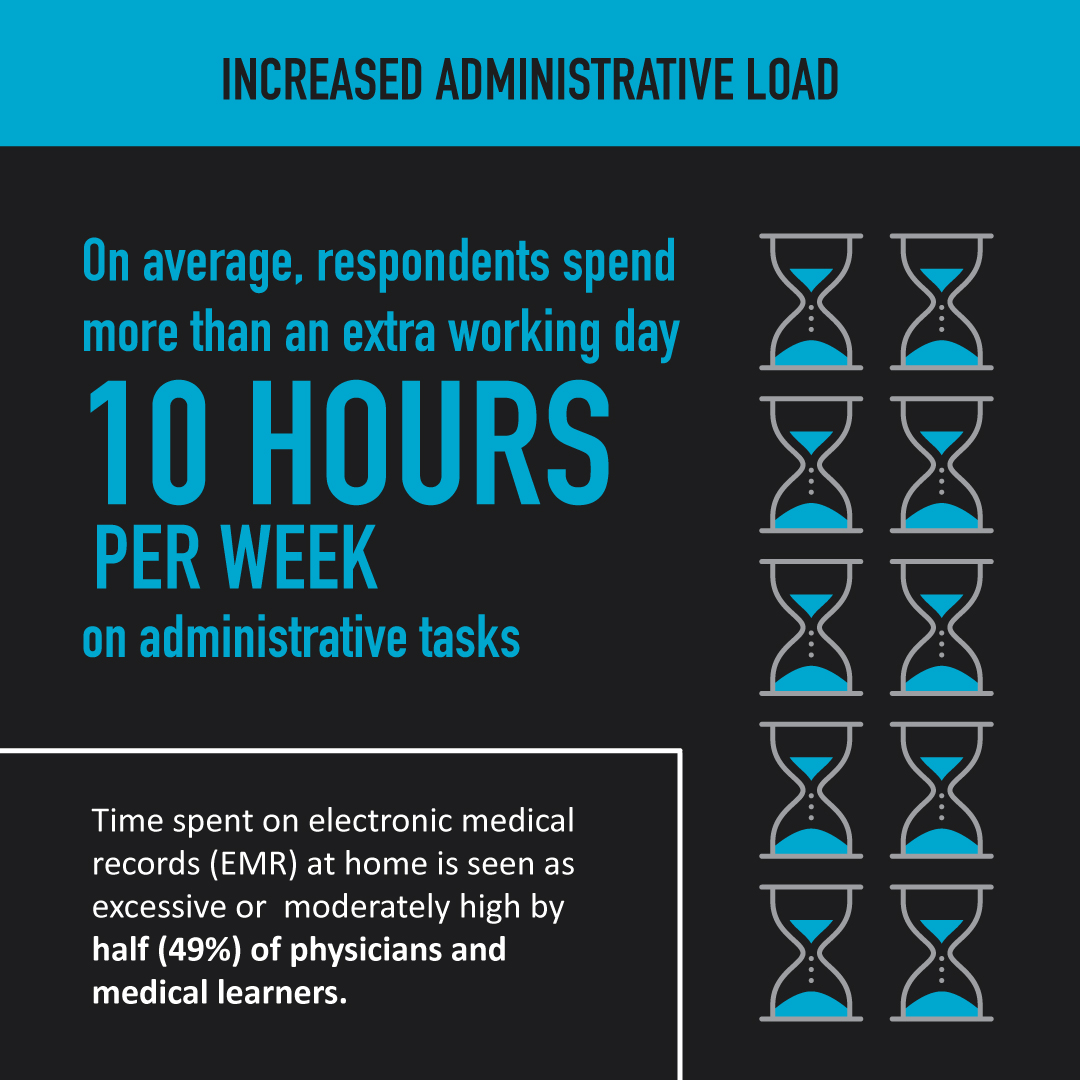
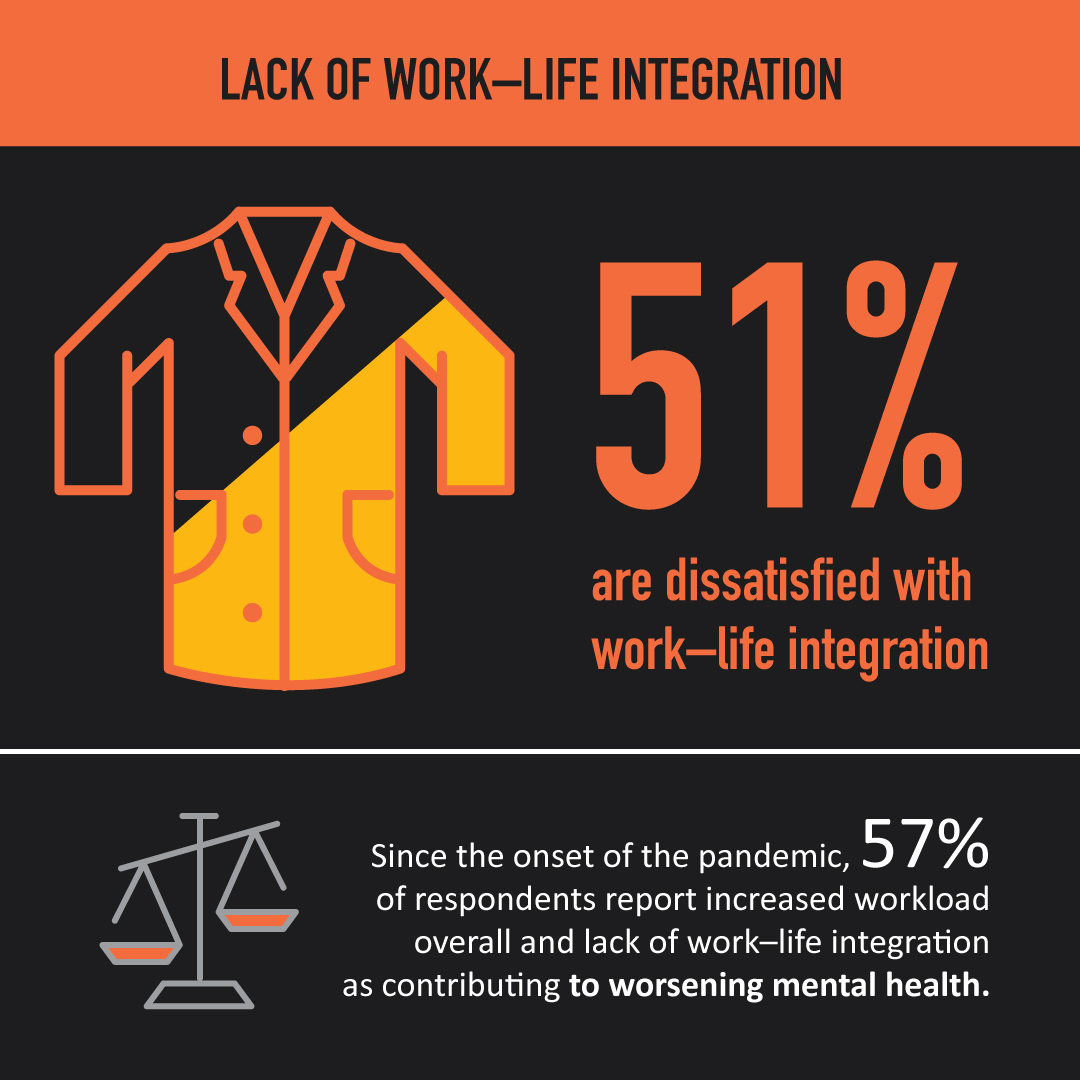
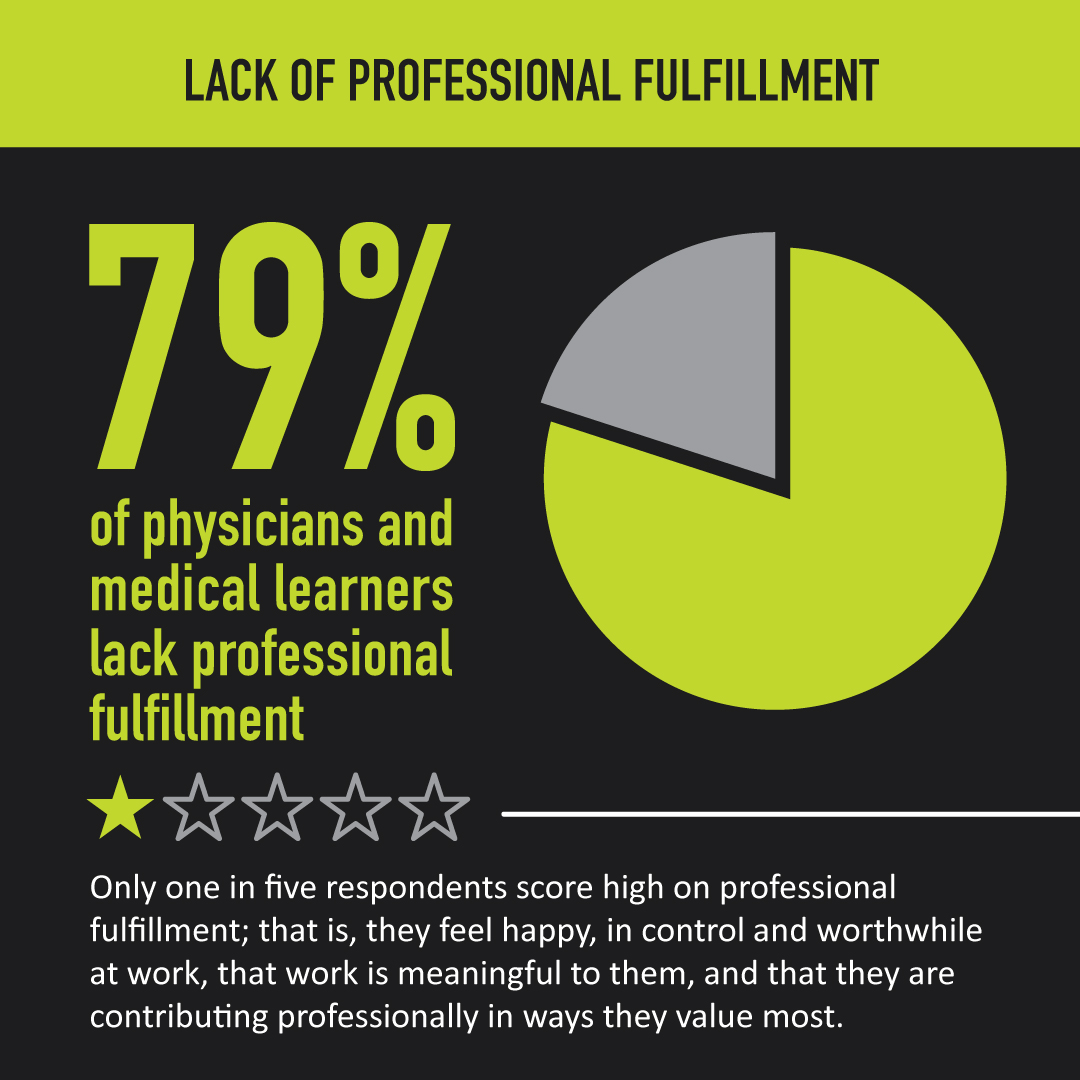
Responses from more than 4,000 doctors, residents and medical students shed light on challenges to physician health and wellness, including lack of work–life integration, bullying and harassment, high administrative burden, lack of professional fulfillment and, of course, the impact of COVID-19.


What is the National Physician Health Survey?
Even before a global pandemic was declared in March 2020, surveys of physicians across the country showed they were at high risk of developing symptoms of burnout, depression and other forms of psychological distress.
Launched by the CMA in 2017, the NPHS is conducted on a three- to four-year cycle to better understand health and wellness among physicians and medical learners. The survey generates an up-to-date and relevant data set that the CMA, as well as other organizations, researchers, educators and stakeholders, can use to inform and advance physician health initiatives.
“The CMA has been ringing the alarm about burnout among physicians and other health care workers throughout the pandemic. This data set — the only one of its kind in Canada — again underscores just how dire the situation is in Canadian health care.” — Dr. Alika Lafontaine, CMA president
Significantly, the study uses an equity lens to examine the health and wellness of specific at-risk subgroups, which will help inform recommendations for system-level changes to improve physician health and wellness — from medical school through retirement.
Who responded to the survey?
From October to December 2021, more than 4,100 physicians, medical residents and medical students completed the NPHS, up from nearly 3,000 CMA members in 2017. The CMA promoted the survey via email to members, social media and advertising and through CMA communications channels including partner organizations to best engage with the larger medical profession.
What did the CMA learn from the 2021 NPHS?
The mental health of physicians and medical learners has continued to deteriorate in recent years, with the COVID-19 pandemic exacerbating existing cracks in the health care system.
Sound Mind podcast: The Great Resignation comes to medicine
Ten statistics highlighting the troubling state of physician health and wellness:
- 60% of physicians and residents indicate that their mental health has worsened since the onset of the pandemic
- Nearly half of respondents (48%) screen positive for depression, up significantly since 2017 (34%)
- One-quarter (25%) of physicians and residents experience severe (10%) or moderate (15%) anxiety
- More than half of physicians and medical learners (53%) experience high levels of burnout
- Nearly half (49%) of respondents are considering reducing their clinical work in the next 24 months
- More than one-third (36%) of respondents have had thoughts of suicide at some point in their lives, and 14% have had thoughts of suicide in the last 12 months
- Moral distress is pronounced among physicians and medical learners, with one in five saying they have felt it “very often” or “always,” and a further 33% saying “sometimes,” since the start of the pandemic
- Nearly half of physicians (47%) report low levels of social well-being — feeling that you have something important to contribute to society, for example, or have a sense of belonging in a community — a proportion that has significantly increased from the 2017 survey (31%)
- Eight in 10 (79%) physicians and medical learners score low on professional fulfillment; less than six in 10 physicians and medical learners indicate being satisfied with their career in medicine
- Results reveal several at-risk subgroups who are experiencing more negative wellness outcomes, including residents, younger physicians, women, those with six to 10 years in practice, parents and/or caregivers, those living with disabilities and those working in small town/rural or isolated/remote areas
Looking ahead
While the 2021 NPHS highlights the challenges physicians and medical learners are facing, some encouraging findings are also worth noting. There are signs of a culture shift toward prioritizing wellness. This includes the finding that medical residents and younger physicians are accessing support for their mental health challenges more frequently than their later career counterparts.
However, significant barriers to seeking help remain for many respondents, who report stigma, availability and concerns around confidentiality. In fact, three in 10 physicians cite confidentiality as a barrier, while 21% identify the risk of losing a medical licence and being unable to practise as a factor in whether or not to seek support.
“Strengthening health and wellness in medicine is a shared responsibility,” says Dr. Lafontaine. “Moving forward, these national survey data will be instrumental in advocating for physicians and making meaningful changes in the culture of medicine.”
In coming months, the CMA will take a deeper dive into the results of the 2021 NPHS to better understand the root causes of physician health and wellness concerns and how best to tackle the challenges facing the medical profession.
