CMA EXPLAINS
What pan-Canadian licensure can do for a workforce in crisis
In Canada, medical practice has been restricted to the province or territory in which a physician is licensed. Other than a few exceptions, practising in a different province or territory has involved a lengthy application process, sometimes months long, and thousands of dollars in fees.
The CMA has been calling on governments to implement pan-Canadian licensure as an important step to better health care.
It could help alleviate the pressure on the medical workforce serving patients in rural and remote communities by making physicians more mobile. It would allow for more efficient responses to delivery of health care, including in crises such as the COVID-19 pandemic. It would also support virtual care across provincial and territorial borders, providing greater continuity and more timely access.
Mobility would provide urgently needed support for physician work-life balance, health and wellness, too, potentially improving retention rates by making it easier for doctors and hospitals to fill locums for holidays, parental and educational leaves.


“It’s no wonder physicians have such high rates of burnout. There’s no such thing as a healthy work-life balance if you’re constantly faced with the decision to either cancel patients and feel like you’ve abandoned them, burden an already overworked colleague with squeezing them in, cancel your vacation (yet again), or show up to work sick and tired.”
Dr. Jordan Vollrath, family physician in AB
Greater physician mobility is gaining momentum. In May 2023, a new Atlantic Physician Registry was launched to allow practice across Nova Scotia, New Brunswick, PEI and Newfoundland and Labrador. In October, federal, provincial and territorial health ministers committed to a new process for physicians in good standing to practise across the country. The CMA welcomed that announcement and continues to advocate for its timely implementation.
How does the CMA define pan-Canadian licensure?
The ability for physicians with full licences to practise independently without restrictions or for medical resident trainees registered in any Canadian jurisdiction to practise or train in any other Canadian jurisdiction without having to acquire more than one licence or pay additional licensing fees.
How big an issue is access to care?

6.5 million Canadians do not have primary care
Patients are having to turn to walk-in clinics and emergency departments. The resulting increased wait times and emergency department overload are overwhelming other parts of the health care system.
Source: Statistics Canada

Only 8% of medical professionals support 18% of Canadians who live in rural or remote communities
Some communities, like Hay River, NWT, have to regularly close emergency departments for indeterminate periods due to staff shortages.

Physicians are under unprecedented pressure: 53% report a high level of burnout
System inflexibility — including the current licensure model and the barriers it creates for locums to support an improved physician work-life balance — is a big part of the problem.
How would pan-Canadian licensure help?

Present reality
In many northern and remote communities, accessing both routine and specialized care can mean flying to large centres for care at tremendous costs to patients, their families and the health system.
Specific medical services may be inaccessible even in communities that are not remote. These patients, too, are forced to take time off work, pay for travel and childcare and leave their support networks for treatment.

Pan-Canadian promise
The same physicians who attend to these patients could deliver many services through virtual care, reducing the frequency and duration of fly-in visits, and providing care to patients whose conditions don’t allow for travel.

Present reality
In most provinces and territories, there’s a shortage of eligible physicians to fill locum positions. In a staffing crunch, this makes it difficult for physicians to provide an appropriate level of care for patients. It also hampers work-life balance, disproportionately affecting female physicians, who may be unable to find coverage for parental leaves.

Pan-Canadian promise
A national pool of eligible physicians to fill locums would allow for greater continuity and quality of care; provide valuable work experience for new physicians; and create greater flexibility in practice, reducing workplace stress.

Present reality
Licensing restrictions make it difficult for patients to cross borders, too. After three months in a new province or territory, they’re no longer covered for care from doctors they’ve left behind – even virtually. Instead, many are forced to join lengthy waitlists for access to local providers, sometimes taking years to find a physician, if one is available at all.

Pan-Canadian promise
Pan-Canadian licensure would help bridge the gap in primary care services for Canadians on the move from one jurisdiction to another, ensuring continuity of care.

“As a PEI resident, critical and specialty cardiac care requires physically going to Halifax or Saint John – six hours round-trip for either location. This means time off work, and out-of-pocket transportation, hotel, childcare and family visitation expenses. My hope for the future would be a scenario where specialists would have the option of serving patients in other provinces through virtual care.”
– Patient Angie MacCaull, Summerside, PEI
There is a will
A 2022 survey of CMA members shows overwhelming support – 95% of respondents – for pan-Canadian licensure.
Improving access for patients



Boosting the health workforce
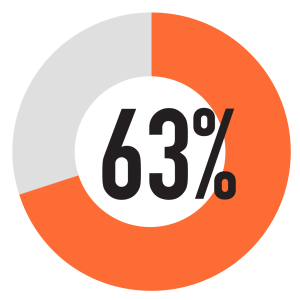
63% said they would be more likely to seek out locum opportunities in other provinces
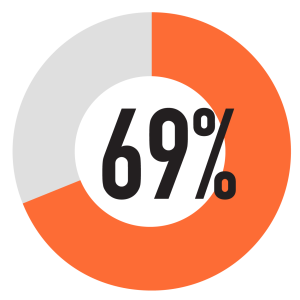
69% said they would be somewhat or very likely to continue to practise part-time during retirement
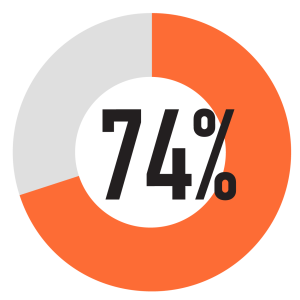
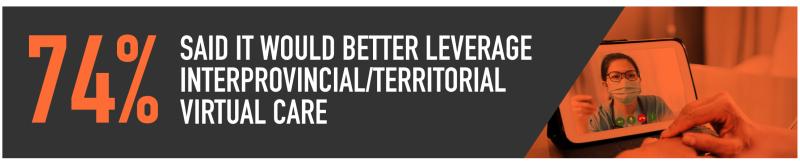
74% said they would be somewhat or very likely to remain in Canada rather than seek opportunities abroad
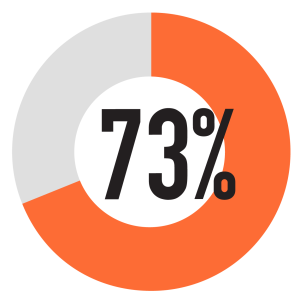
73% said it would make Canada more attractive to international medical graduates
There is a way
In 2010, Australia adopted all-jurisdiction licensure for a broad range of health care practitioners. Each profession has a national board which regulates and registers practitioners, and develops standards, codes and guidelines. This approach ensures standardized high-level medical competence and quality of care while making it easier for health professionals to work across different states — in person and virtually. Since implementing all-jurisdiction licensure, there’s consensus that the new system is working well and has led to significant improvements in terms of workforce mobility, patient safety and better data for workforce planning.

Faced with a health workforce crisis, why is the CMA making pan-Canadian licensure such a priority?
The CMA is pressing for this solution as a partial response to the health workforce crisis.
The CMA continues to call on governments to consider pan-Canadian licensure as one step in addressing excessive wait times, cross-border virtual care and widespread family physician shortages, and in filling locums to support the health and well-being of doctors everywhere.
What can I do to help? Continued physician and public support for pan-Canadian licensure is critical to making it a reality. Together, we have an impact. Find out how to get involved with the CMA’s work, today.
Quotations have been edited for clarity and length.

