There aren’t enough family doctors to go around.
More than 6.5 million Canadians do not have regular access to primary care. One-third of Canadians who have a family doctor find it difficult to get an appointment.
Physicians themselves are experiencing exhaustion, burnout and job dissatisfaction. In a May 2023 survey by the Ontario College of Family Physicians, 65% of respondents cited plans to leave office-based family practice or reduce their hours in the next five years.
At the same time, there’s declining interest in family medicine as a specialty. In July 2023, there were almost 1,000 unfilled positions for family physicians across the country.
More than a straightforward numbers game, the primary care gap reflects a changing field. Patients have more complex, chronic conditions. There are more diagnostic tests to consider. And many procedures and treatments have shifted from hospital settings to community-based care.
Family practice now includes patient navigation, interprofessional coordination and a greater administrative burden. All of which, simply put, takes more time.
“We cannot simply recruit our way out of this problem. We need to modernize how primary care is delivered to reflect the evolving needs of our population and those providing the care.”
– Dr. Kathleen Ross, CMA President
Team-based primary care is one way to do that.
With the proper resources and organization, inter-professional health teams allow providers to focus on the work they do best, improving job satisfaction while giving more patients the right care at the right time.
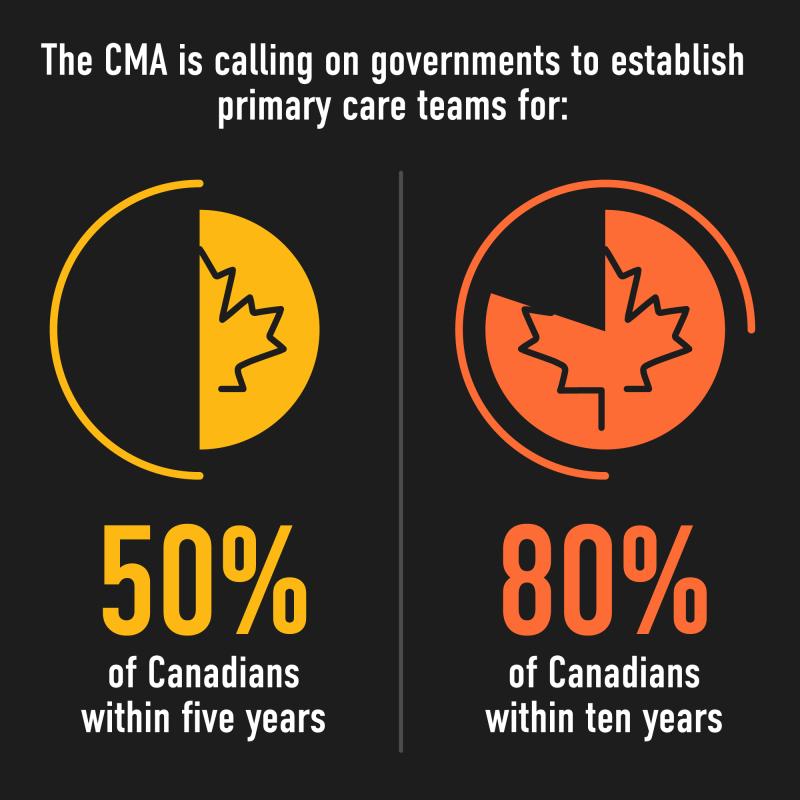
That’s why the CMA is calling on governments to establish primary care teams for 50% of Canadians within five years, and 80% within 10.
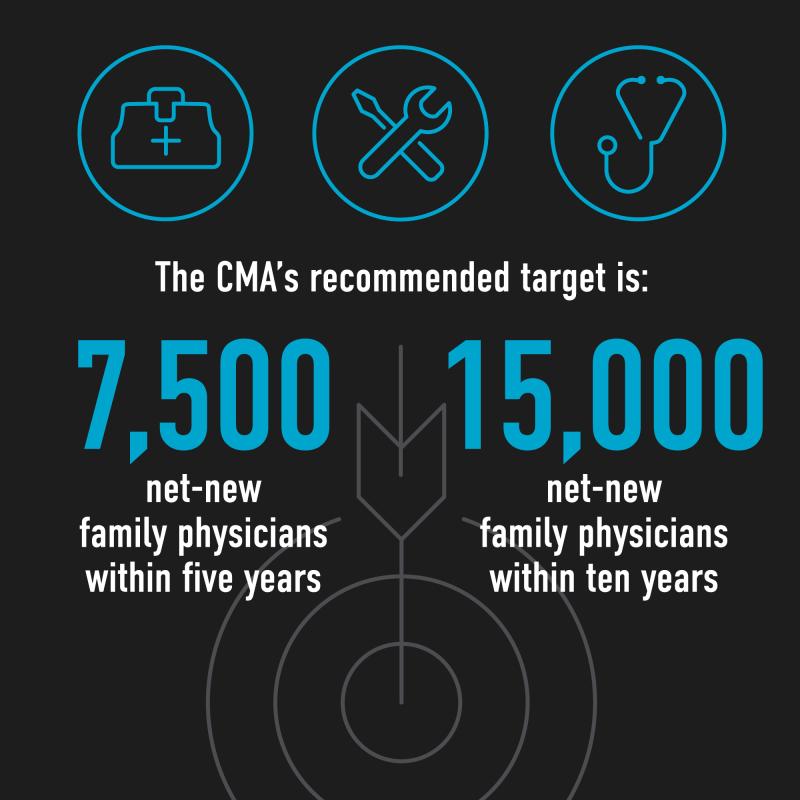
Training and recruiting more family doctors is still needed. The CMA’s recommended target is 7,500 net-new family physicians within five years, and 15,000 within 10.
The supply of other primary care providers, including nurse practitioners, nurses, and physician assistants, will need to increase in tandem.
But as Dr. Ross puts it, “It’s about making the bus go faster. By leveraging the skill set of every health professional on the team, we have the collective ability to see more patients and to ensure they are getting the most optimal care from the provider best able to meet their needs.”
Team-based care in Canada
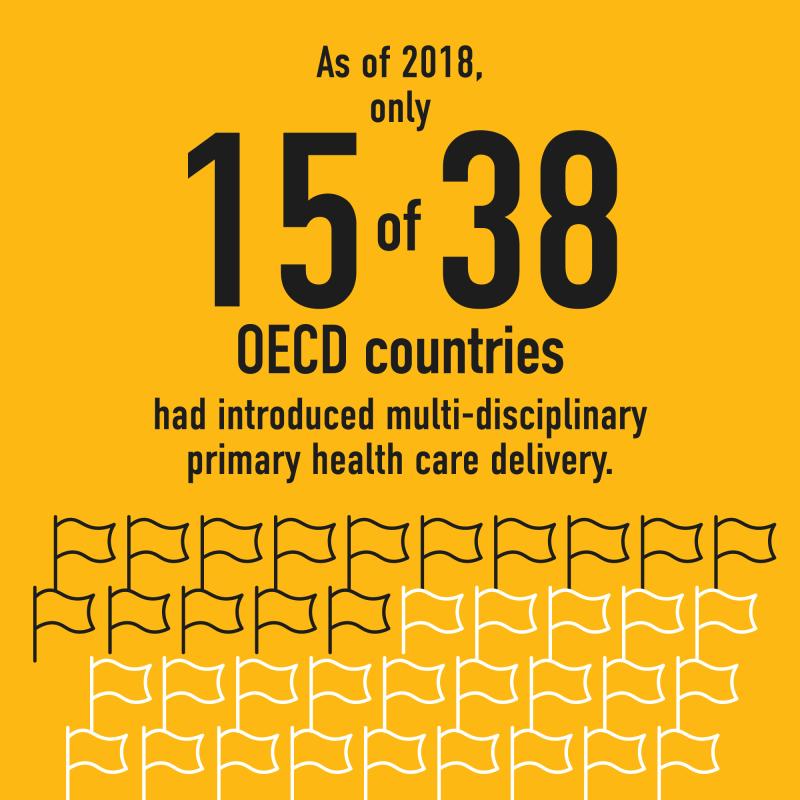
There are different models and names for team-based primary care: Primary Care Networks in Alberta, Family Health Teams in Ontario and Family Medicine Groups in Quebec. Each is redefining how care is delivered. And more provinces are seeing teams as a viable way to expand access to primary care.
What different health teams have in common is a broad range of services offered by a well-connected interprofessional team, including virtual care and referrals. The team might not be located under the same roof, but the patient is always seen by a professional with relevant skills who can connect with a physician as necessary.
At a national level, the College of Family Physicians of Canada introduced a vision for patient-centred, continuous, comprehensive and accessible primary care called the Patient’s Medical Home in 2011.
In its 2023-24 budget, the PEI government pledged $8.9M to add more Patient’s Medical Homes across the province and hire 100 new positions to support current and future medical homes.
In September, New Brunswick announced it will turn to collaborative care practices — offices where multiple health practitioners work together to service a large pool of patients — to address a growing population and a shortfall in primary health care professionals.
Who should be part of a primary care team
At the 2023 CMA Health Summit session on Scaling up Team-based Care, participants were asked who should be part of a primary care team:
Most clinicians agreed that having someone who can reduce physicians’ administrative burden by handling patient navigation, referrals, writing prescriptions, ordering tests, etc., was imperative. Beyond that, they stressed that who belongs on a team depends on the patient population. For example, if there are many older adults, a team may need a nurse with expertise in gerontology. Supporting culturally safe care is another critical consideration.
Patients said that which team member delivers their care is less important than the goal of improving access and getting their health information in a timely manner, whether in person, by phone or electronically.
Who I want on my primary care team
Dr. Tara Kiran, a family physician and researcher in Toronto, is leading OurCare, a national project on primary care. In a survey of 9,000 Canadians, 90% of OurCare respondents said that, in addition to a family physician, they’d be willing to see a nurse practitioner for most of their needs. Who else do they want on a primary care team:
The benefits of primary care teams
For patients
Not every problem needs to be seen by a family doctor. Allied health professionals have the skills to assess, treat and connect patients to programs in their community — faster.
Because patients in primary care teams are seen by a broad range of health professionals — including, in some cases, pharmacists, physiotherapists, and even chiropodists — they often have better continuity of care as well.
“Safe care happens with teams. Having that supportive culture where everybody, including patients and families, shares the decision-making and feels comfortable speaking up, is an important foundation for the future success of the health care system.”
– Teri Price, Patient partner and executive director of Greg’s Wings Projects
For providers
Team-based care allows every professional on the team to work at the top of their scope of practice and facilitates efficient collaborations to meet patients’ needs. Doctors might develop a rehabilitation plan with a team physiotherapist, for example, or conduct a medication review in consultation with a team pharmacist. Team members also share the patient load and can provide coverage when others are sick or need time off.
Listen: Sound Mind podcast – The wellness benefits of team-based care
For the health system
Connecting more people in Canada to primary care teams and their focus on disease prevention and management will help alleviate many downstream issues, including overcrowding in hospitals and pressure on emergency departments.
For example, Dr. Kiran found that, while emergency department visits have been increasing for all patients in Ontario, patients who were part of a team had a lower increase in emergency department visits over time.
Teams can also strengthen relationships with specialists and community supports like home care and mental health and addictions counsellors and support cultural safety in care.
Ultimately, primary care teams can help patients the access care they need, whenever they need it.
In a 2017 review of research on practices aligned with Patients Medical Home:
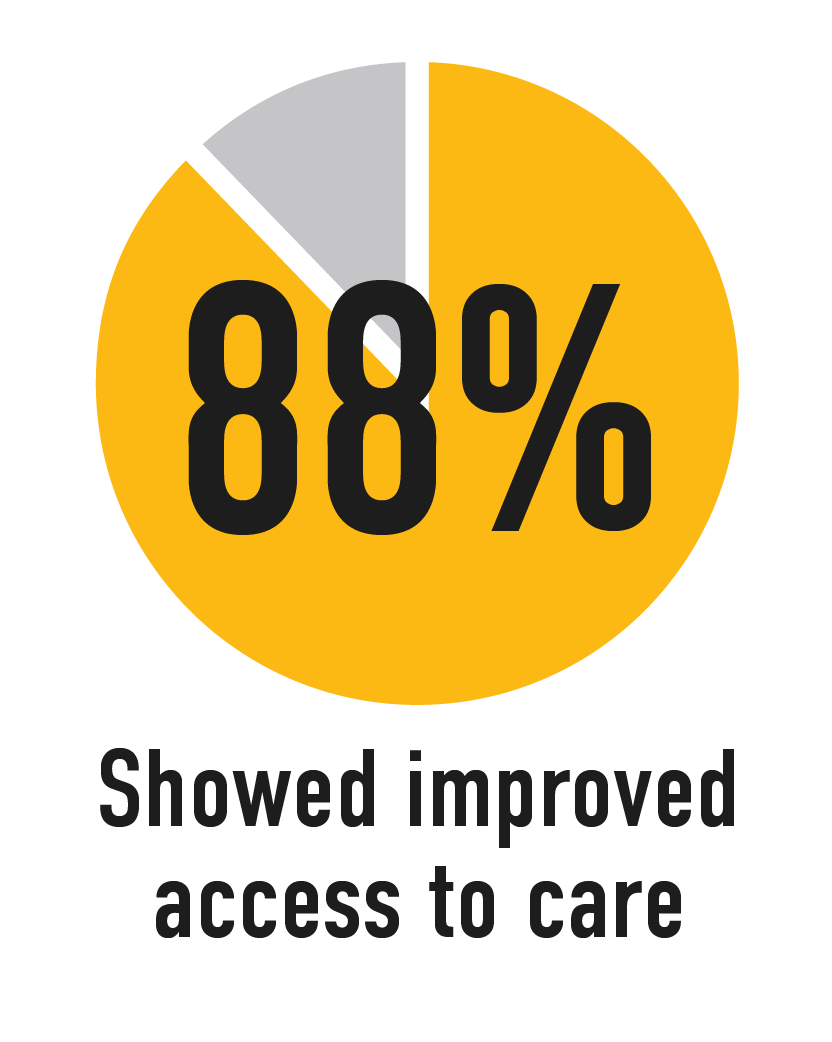
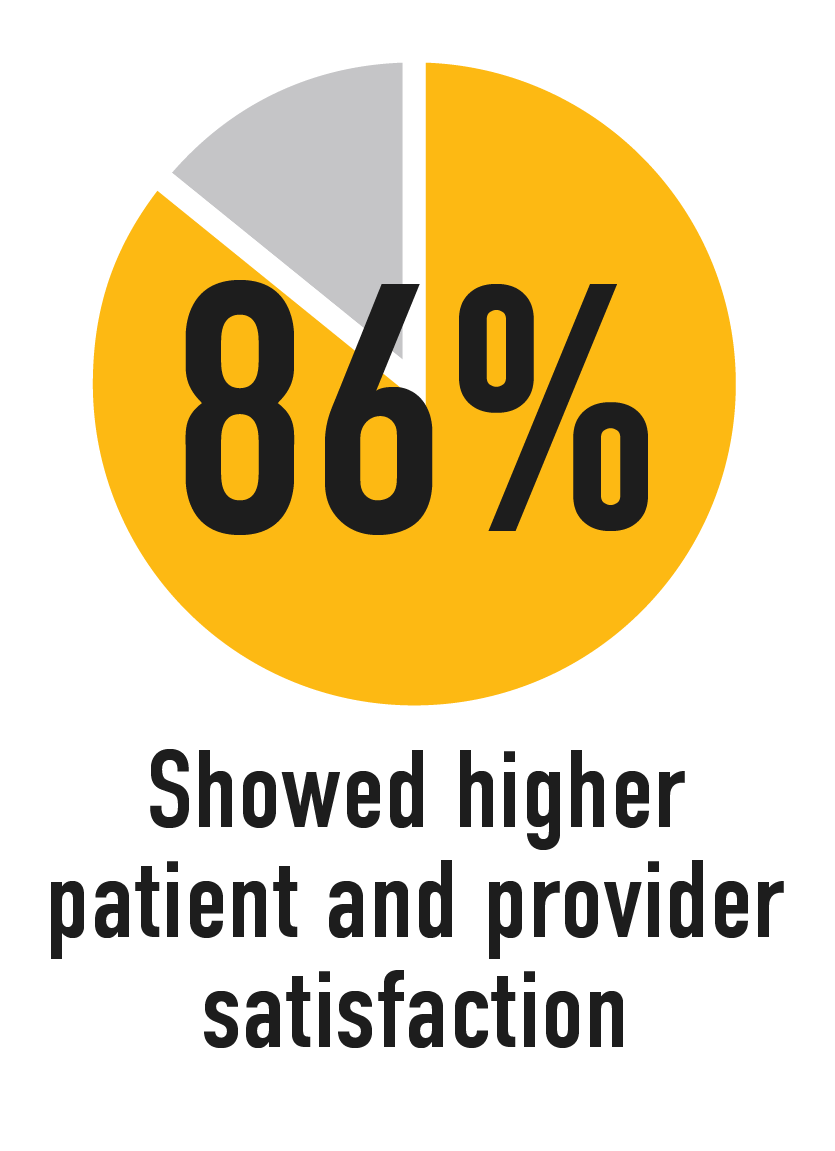
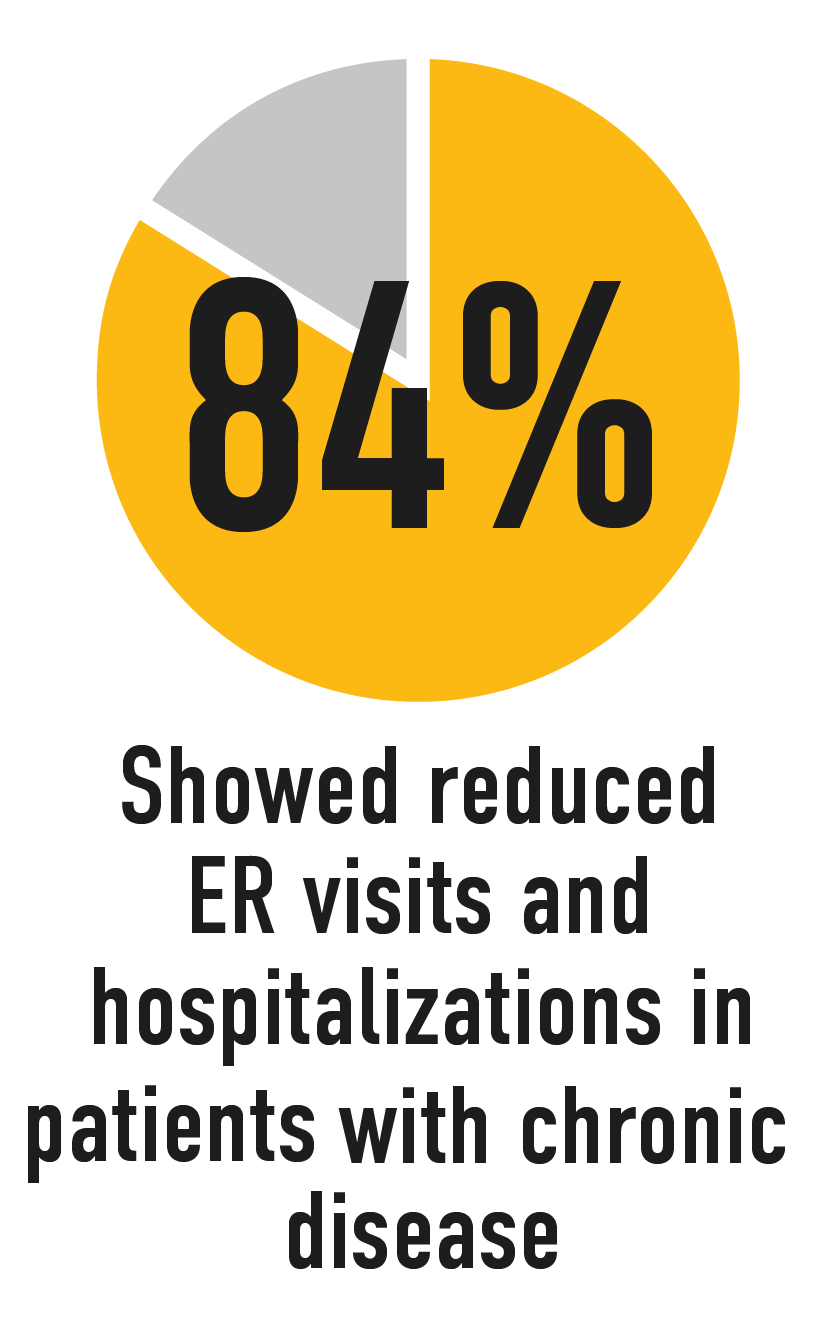
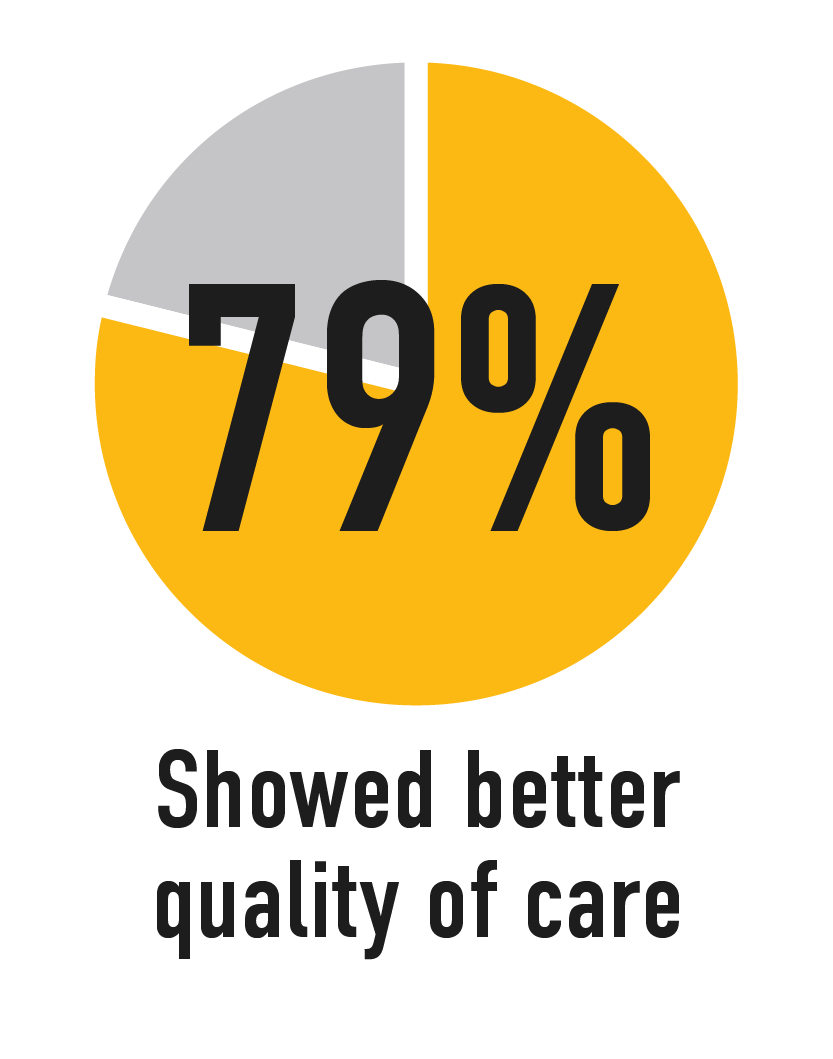

Source: Patientsmedicalhome.ca
What the CMA is doing to support team-based primary care
The CMA is calling for scaled-up team-based care as part of broader support for primary care at a national level.
The most recent federal-provincial health agreements included mandatory progress reports on “headline” indicators to improve accountability in health care. The CMA has urged governments to adopt further targets specifically tied to both primary and team-based care.
This work builds on eight recommendations for Ottawa to alleviate the health workforce crisis developed in partnership with the Canadian Nurses Association (CNA) and the College of Family Physicians of Canada (CFPC). One critical call to action is leveraging the federal government’s $3.2 billion commitment to a Primary Care Integration Fund to expand the Patient’s Medical Home model. These joint recommendations were also presented to the Federal/Provincial/Territorial Committee on Health Workforce.
The CMA continues to engage physicians, patients and policymakers on team-based care. Feedback from workshops held at the 2023 CMA Health Summit, for example, will help us build a framework for scaling up primary care teams.
What you can do to help
Physician and public support for expanded team-based care is critical to making it a reality.